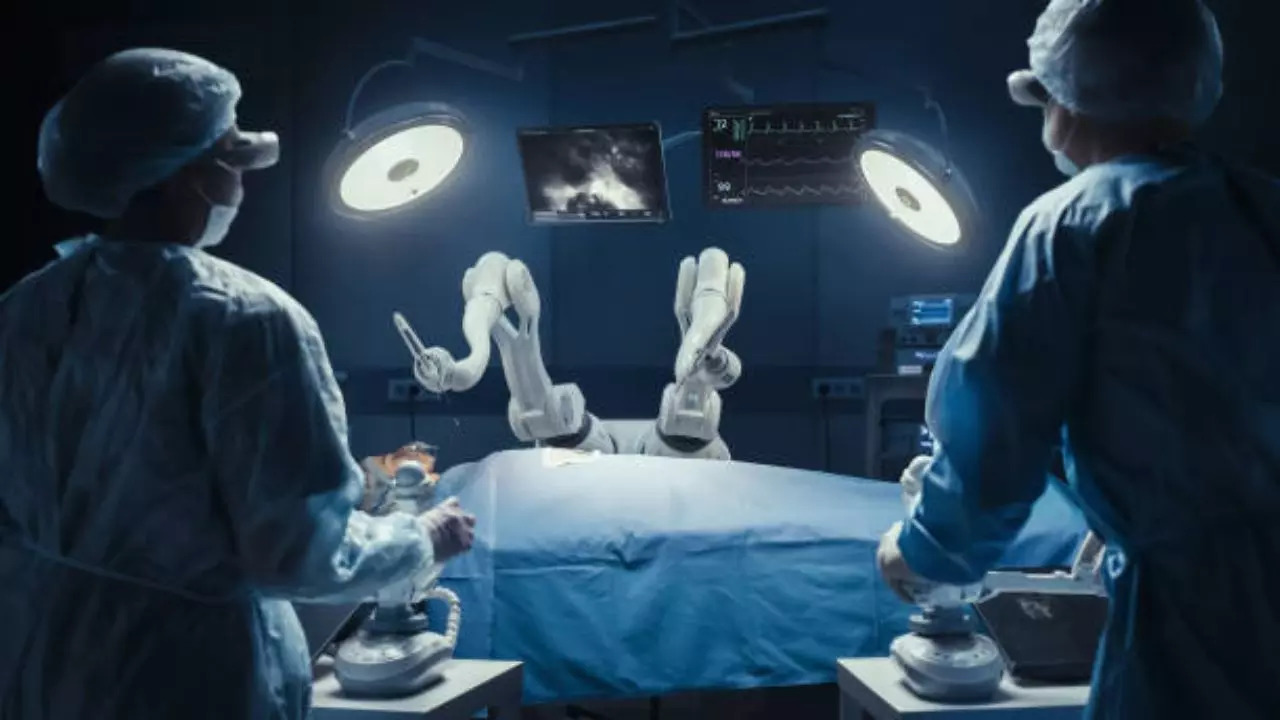
Doctors perform India’s first scarred ectopic pregnancy using robotic surgery (Image credit: iStock)
The first from India Ectopic pregnancy with scar A 44-year-old woman underwent robot-assisted surgery. A team of doctors led by Dr. Aruna Kalra, Director, Obstetrics and Gynecology, CK Birla Hospital, Gurugram, performed robot-assisted surgery and helped the patient successfully deliver a healthy baby. The incidence of mortality in ectopic pregnancy It is 5 to 10 percent. If action is not taken in time, before an imminent rupture occurs, there is a high probability of mortality due to hemorrhagic shock syndrome and abnormal blood clotting in all blood vessels of the body, leading to multiple organ failure.
On admission to the hospital, the patient was suffering from severe abdominal pain and low blood pressure. An ultrasound scan showed an imminent rupture of the uterus at the site of the scar. The woman had tried to get pregnant several times in the past but had not been successful. When she first became pregnant in 2014, the baby was found to have a spina bifida abnormality (inadequate development of the baby’s spine and spinal cord, causing a gap in the spine) at 28 weeks. A caesarean section was performed, but the baby died inside her womb. She subsequently tried to conceive again, but her tubes were blocked and she was unable to conceive naturally.
She eventually underwent in vitro fertilization (IVF), but the result was an ectopic pregnancy. pregnancy in the isthmocele at the site of the previous caesarean scar. The scar from an ectopic pregnancy would have ruptured as it continued to grow and was therefore removed with robotic-assisted surgery. Eventually, the woman conceived again and this time it was a successful IVF pregnancy; the scar was not affected because it was sutured in a double layer at the time of robotic surgery. A full-term caesarean section was performed and she gave birth to a healthy baby.
In this case, robotic-assisted surgery was chosen because the ectopic pregnancy scar is located in the lower uterine segment, very close to both uterine vessels supplying the uterus, making this area risky to operate on. The urinary bladder is attached to the ectopic pregnancy site, making dissection extremely delicate and difficult. The risk of inadvertently cutting blood vessels in an already compromised patient may be pathological. Blunt dissection to separate the bladder may perforate it if performed with any instrument other than thin, flexible robotic instruments with a magnified view of the adherent tissue planes between the uterus and bladder.
Postoperative complications are very common in this surgery, leading to a poorer recovery. These surgeries are successful if the surgeon is skilled in the robotic technique and the result is wonderful, with no blood loss, no tissue injury, no complications and no secretions on the same day. The strength of the sutures ensures that the patient will be able to carry a pregnancy after 3 months of surgery.
Explaining the case in detail, Dr Aruna Kalra, Director of Obstetrics and Gynaecology at CK Birla Hospital, Gurugram, said, “This is a rare case of scar pregnancy, which occurred following a previous C-section. As we repaired the scar using a robot, it was quite easy to deliver the baby this time. The incidence of scar ectopic pregnancies is increasing due to the rising rate of C-sections, which are now the most common surgical procedure performed worldwide.”
“A ruptured ectopic pregnancy is a catastrophic condition that causes a blood loss of 2 to 3 liters into the peritoneal cavity. The patient was diagnosed and operated on just in time to prevent the rupture of the uterus, which could have cost her life. Ectopic pregnancy is a cause of maternal mortality during the first trimester of pregnancy, with a rate of 9 to 14 percent and an incidence of 5 to 10 percent of all pregnancies. The cause of death is hemorrhage and shock syndrome (multiple organ failure due to disseminated intravascular coagulation, abnormal blood clotting in all blood vessels of the body). In addition, an increase in the rates of scarred pregnancies and isthmocele may be a result of this increasing prevalence of cesarean deliveries. This phenomenon, known as scarred ectopic pregnancy, is very rare and occurs in about 1 in every 1,500 to 2,000 pregnancies, however, the prevalence is increasing,” he explained.
What is an ectopic pregnancy?
An ectopic pregnancy occurs when a fertilized egg implants and grows outside the main cavity of the uterus. While in many cases ectopic pregnancies resolve on their own and the pregnancy tissue passes out of the cervix on its own, in many cases it creates problems around the sixth week of pregnancy. 1 in 100 pregnancies are ectopic and are considered an emergency for the pregnant woman. They may not be detected by patients or doctors and if not treated in time, could be life-threatening.
Disclaimer:
The information contained in this post is for general information purposes only. We make no representations or warranties of any kind, express or implied, about the completeness, accuracy, reliability, suitability or availability with respect to the website or the information, products, services, or related graphics contained on the post for any purpose.
We respect the intellectual property rights of content creators. If you are the owner of any material featured on our website and have concerns about its use, please contact us. We are committed to addressing any copyright issues promptly and will remove any material within 2 days of receiving a request from the rightful owner.